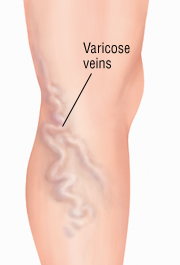
We often hear from patients that are concerned about their varicose veins, but not sure if they are problematic. It’s very common to wonder when to start worrying about varicose veins.

Varicose veins are not normal. If you look at a child’s leg, its very rare to see varicose veins or even many veins at all. All varicose veins are abnormal and represent veins that have lost normal function due to a loss of normal venous valve function. But not all visible varicose veins need to cause concern.
Understanding when and when not to worry can be helpful as people determine if they need to be seen by a vein specialist for help.
Schedule a Consult for Varicose Veins >>
Why Do We Get Varicose Veins?
All veins have valves to help promote blood return from the heart from the legs. The veins are like an upside down tree with lots of branches in the lower leg and more and more larger vein branches as the veins get to the pelvis.
Once the veins cross into the pelvis there are two main vein branches know as the iliac veins. Below most the veins have valves so that when the patient walks and moves the muscles squeeze and push the blood up. The valves keep the blood from coming back down.
There are two main systems in the leg. One is the deep and the other is the superficial. Most of the blood comes up the deep veins. Varicose veins are primarily from valve dysfunction in the superficial veins. The primary superficial veins that impact the development of varicose veins are the saphenous veins and its branches. Such when people have varicose veins most of the time its from failure of the valves of the saphenous veins (which are just below the skin).
Ultimately the main cause of impaired valve function in the saphenous veins is usually genetic. This is called primary venous insufficiency. Or in some cases it can be damage from prior clots (like DVT or phlebitis after injuries or trauma). This is called secondary venous insufficiency.
Ultimately the cause does not matter much as people do not have much control over either by the time the varicose veins develop.
When is Worrying about Varicose Veins Justified?
Some people simply see varicose veins but they have no symptoms from them. Symptoms include pain, swelling, ache, skin changes or wounds. These are called asymptomatic varicose veins. When they are asymptomatic they do not necessarily have to be treated. However, the data suggests that over time, they generally will get worse and at a later date they may become symptomatic. Nevertheless, it is not generally felt by experts that asymptomatic varicose veins need to be treated for medical purposes or to prevent progression.
Sometimes patients wish to have varicose veins treated for cosmetic concerns. This can be done.
On the other hand, many people start to worry once they start to have symptoms. Typical symptoms include ache, swelling, tenderness along the veins and skin changes or blood clots (known as phlebitis). Ache, swelling, and tenderness or throbbing are usually the earlier symptoms. A lot of times the patients will say their legs feel heavy or tired. This is because there is extra blood that is pooling in the legs.
More advanced symptoms include skin changes, such as ankle discoloration or stasis dermatitis. Another advanced complication is blood clots in the veins, known a phlebitis.
Finally, skin changes such as ankle discoloration can occur where the skin becomes red, irritated, brown and itchy. The ultimate stage of this is bleeding from the veins or wounds that open that do not heal. This is known as venous stasis ulcers which occurs when the skin is so damaged by the foot and ankle it cannot heal.
Any symptoms of these nature are worthy of concern and can be addressed in a vein evaluation consultation with a vein specialist. Most are gradual and can be addressed in a elective fashion. But if you have new signs of swelling, redness, hard spots, bleeding or wounds you are best to seek attention promptly if needed.
What Can be Done to Treat Varicose Veins?
The good news is there are numerous treatment options that can significantly reduce symptoms and improve overall vein health. Nearly all can be done in the out patient office setting in quick procedures with little or no downtime.
If you are interested in learning more about varicose veins treatment options, simply fill out our Online Appointment Request Form or call any of our clinics in Northwest Portland , Tigard, Happy Valley, Hillsboro or Bend, Oregon.
