What is a DVT?
DVT, or deep vein thrombosis, is a blood clot in the large veins of the legs (most commonly) or less commonly the arms.
The general function of the cardiovascular system (heart, lungs, and blood vessels) is to deliver oxygen and nutrients to the cells of the body. The heart pumps the blood through arteries to supply oxygen and other nutrients to the tissues throughout the body. Veins are needed to carry deoxygenated blood back to the heart and lungs.
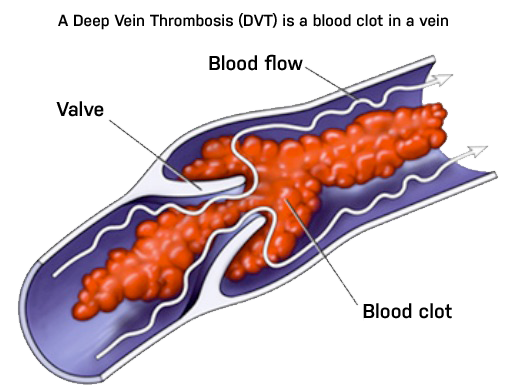
The blood from the legs must make its way against gravity back to the heart. This is done by a series of veins that have valves in them to prevent back flow of blood. As the leg muscles move, the blood is squeezed up the veins, and the valves keep the blood from flowing back down with gravity.
The veins start as a series of small parallel passages that join to form progressively larger veins, which in turn join larger and larger veins until they meet the Inferior Vena Cava, which is the largest vein in the body. The inferior vena cava is connected to and drains to the heart, where the blood is again pumped through the lungs and then is sent back out to the arteries.
The venous system to the lower part of the body can be viewed as an upside down tree, with smaller branches joining larger and larger branches until they join the inferior vena cava, which is like the tree trunk. The veins next to the skin are called superficial veins, and the veins deep to the muscle are called deep veins. The deep veins carry the majority of blood out of the leg.
A clot in the deep veins can be a serious medical condition. Another way to look it this is to think of the veins in the legs like a highway system. The deep veins are the main south to north interstate system heading to main destination (the heart). This interstate highway (deep vein) has more traffic (volume) and travels at a higher speed (pressure).
All the state highways and side roads that feed into the interstate are like the superficial veins. These have less volume and lower pressure. Eventually all roads lead back to the heart.
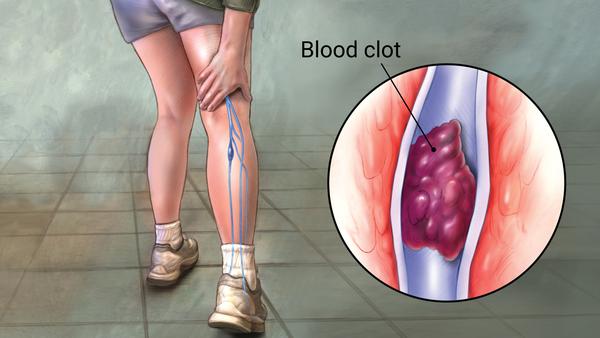
On a highway, what happens when there is an accident on the main interstate highway going north? Of course this can lead to a massive traffic jam. In the veins, this blockage can result in a pressure build up, and ultimately re routing of flow around the blockage. When this happens in the veins due to a clot in the deep veins, it is called a deep vein thrombosis, or DVT.
What causes DVT?
There are a number of reasons why clots can form in the deep veins. Long ago it was recognized that clots form in veins for three basic reasons which are (1) damage to the vein wall; (2) lack of blood movement (also called stasis), and; (3) a pre-disposition to form clot called hypercoagulibity.
- Damage to the vein wall
Damage to the veins can happen in a number of settings, including recent surgeries, accidents and falls or other types of trauma. Injury to the vein is a very common cause of DVT. - Lack of blood movement (stasis)
Stasis occurs when a person is immobilized for any number of reasons, including sitting in an airplane or car for long periods of time without movement, or having your leg in a cast. - A pre-disposition to form clot called hypercoagulibity
Finally, and perhaps the least well understood, is hypercoagulability. There are certain people who for one reason or another simply have a predisposition to form blood clots. Sometimes this is due to a very subtle genetic defect where there body does not have the right balance of coagulation factors that either create or more likely, break down clot once it occurs.1 In addition to genetic factors, some patients can develop an acquired propensity to form clot. This is very common in some types of cancer, as well as after surgery or trauma.
Due to a combination of these factors, DVTs are common after certain types of surgery, especially any operation in the abdominal, pelvis, and the legs. This is especially true after orthopedic surgery, where the DVT rate can be as high as 40%.
For example, after many types of surgery, there is a variable combination of injury (from the surgery itself), stasis (from being immobilized during and after surgery) and hypercoaguabity (due to an acquired imbalance of natural coagulation factors) that make the risk of a DVT a not uncommon event after certain operations. For this reason, there are a number of efforts undertaken to try to limit DVTs after surgery.
This effort, called DVT prophylaxis, includes the use of low dose injectable blood thinners, intermittent pneumatic compression devices (leg squeezers), elastic compression stockings and early ambulation, all of which are designed to reduce the chance of a DVT at the time of surgery. Unfortunately, although the risk can be reduced, at this time it is impossible to reduce the risk of a DVT to zero.
How common are DVT’s?
Many people are surprised to find out how many people have a DVT each year. In the U.S., approximately 2 million patients are found to have a DVT and 600,000 patients with a DVT diagnosis will be hospitalized each year. And it is estimated that only half of people with DVT’s are actually diagnosed, meaning many people have a DVT and don’t even know it.
Unfortunately, up 200,000 people die each year due to the complication of deep vein thrombosis, mostly due to pulmonary embolism. Amazingly, many of these deaths could be prevented. DVTs are more common in individuals with risk factors.
Common risk factors for DVT include:
- surgery
- hospitalization for acute medical illness
- nursing home confinement
- trauma
- active cancer
- neurologic disease with paralysis
- varicose veins
- central venous catheters
- pacemaker (because the leads are in the deep arm veins)
Among women, there are additional significant DVT risk factors:
- oral contraceptives
- pregnancy (and immediately after pregnancy)
- hormone replacement therapy
- Also, a PE is the leading cause of maternal death associated with childbirth.
DVT has been associated with travel such as long air plane flights, a condition termed the “economy class syndrome.”
Frequently Asked QuestionsDeep Vein Thrombosis
-
-
What happens if a DVT goes untreated?
Occasionally patients are told they had a prior DVT and they were unaware of the problem at the time. The larger the DVT, the higher the risk without treatment. Thus seeking evaluation any time there is concern for an undiagnosed DVT is advised.
-
Can DVT be life threatening?
Yes, a DVT can be life threatening – especially when it goes untreated. If there is ever a concern a DVT might be present, it is best to seek medical attention.
-
How serious is Deep Vein Thrombosis?
A DVT is a serious medical condition. However, not all lead to long term disability or death. A DVT can range from small, in the calf muscles, and barely noticeable, to large, in the larger veins in the thigh and pelvis. The larger DVTs in the upper leg are more of a risk to break off and travel to the lung (known as a pulmonary embolism, or PE). This can be fatal or very debilitating.
-
Is DVT always fatal?
DVT is not always fatal. Most DVTs can be diagnosed and treated without significant disability to the patient. However, in some cases, unfortunately, a DVT can be fatal. This is usually when it goes unnoticed and becomes quite large in the upper veins in the legs. Then if the clot breaks off it can travel to the heart causing a blockage of the blood flow through the heart and lungs. This is known as a pulmonary embolism (PE).
-
What is the most serious complication of DVT?
In the short term, the biggest concern with DVT is that it can break off and travel through the veins, through the heart and to the lungs. This is called a pulmonary embolism (PE). Rarely, a blood clot can go through a hole in the heart to the arterial circulation, leading to a stroke. This is known as a paradoxical embolism. In the long term, DVT can lead to the Post Thrombotic Syndrome (PTS). This manifests in about a third of patients as swelling, heaviness, brown skin by the ankle, varicose veins and possibly venous stasis ulcers.
-
Can walking dislodge a DVT?
Before a DVT is treated, dislodging is a concern. Once a DVT is diagnosed and treated with anticoagulation, such as Xarelto or Eliquis, the risk is greatly reduced. Once the DVT is treated, in fact, movement is encouraged as it helps blood flow in the legs. However, given that there are some specific considerations for every patient with a DVT, its best to check with the provider treating your DVT.
-
What are the risk factors for DVT?
Veins require movement to optimally function. So when a patient is injured, sick or has surgery, they are not moving as well - and the risk of DVT goes up. This is the same for long distance travel when one does not move their legs over the course of hours. Cancer is a risk factor for DVT. Finally, some people have genetic or acquired blood clotting disorders that make them more prone to DVT.
-
What foods should you avoid if you have DVT?
A healthy diet is important for vein health in general. While there aren’t any specific foods that are known to contribute to DVT, being overweight tends to make vein problems worse. Also, certain foods are known to be inflammatory for certain patients. Vein conditions like DVT involve inflammation and when foods contribute to that, vein symptoms can be worse. In the old days, some patients were treated with Coumadin/Warfarin. These drugs have certain foods that are to be avoided, like green leafy vegetables. But if a DVT patient is on one of the newer drugs, like Xarelto or Eliquis, there are no foods that need to be avoided.
-
How is DVT prevented?
There are certain circumstances when DVTs are more common, like after injury, surgery or travel. Movement, like walking, is important, and in some cases compression stockings will help. After surgery and injury, when one cannot move as well, sometimes medications in pill or injection form are used for DVT prevention.
-
Can DVT go away on its own?
A DVT can range from small to large. Some small DVTs in the calf might fade away without being treated with anticoagulation. The larger DVTs, involving the larger veins in the thigh and pelvis, will not generally go away and need to be diagnosed and treated. If not, untreated DVTs can be life threatening.
-
What are the warning signs of Deep Vein Thrombosis?
Most of the time, a patient with a DVT will have new leg swelling, especially in the calf and around the ankle. They may have lower leg redness and warmth as well as pain in the calf and possibly the thigh. If you are concerned you might have a DVT, it’s important to seek a medical evaluation.
-
About Inovia Vein Specialty Centers
At Inovia Vein Specialty Centers we are leading vein doctors who specialize in caring for patients with venous disorders such as varicose veins, deep venous thrombosis, and venous stasis ulcers. Founded in 2006, we have specialty vein clinics across the Pacific Northwest. Call today to schedule a vein consultation at any of our locations.



