Understanding Varicose Veins in Cancer Patients:
1. Introduction to Varicose Veins
People often ask: What is the connection between varicose veins and cancer? Varicose veins occur when the valves within the veins become weakened or damaged, leading to blood pooling and leg discoloration. Varicose veins are very common in the general population. So it is no surprise that sometimes patients with varicose veins are also diagnosed with cancer.
While varicose veins are commonly associated with aging and lifestyle factors, cancer patients may also experience these enlarged veins with faulty valves due to various factors related to their vascular issues. Some have the varicose veins before they are diagnosed with cancer and others develop varicose veins after their diagnosis and treatment for cancer.
In some cases it is cancer itself that makes patients prone to blood clots or vein issues and at other times it is the cancer treatments including surgery that can make a patient prone to develop blood clots or vein problems.
2. The Connection Between Varicose Veins and Cancer
The presence of cancer cells in blood and the treatments for cancer can affect the vascular system clotting system. For example, cancer treatments such as chemotherapy can alter blood flow or blood vessels and contribute to the development of circulation issues. Further, some patients with cancer develop blood clots in their legs or a blood clot in their lungs (a PEand that can result in the eventual breakdown of valves that later present as varicose veins or spider veins on the legs. Patients with a known family history venous diseases or of blood clots or blood clotting disorders may be more at risk. However, most commonly, the situation is that a patient with long standing varicose veins is diagnosed with cancer and thus they are associated, but not causal so to speak.
3. Understanding the Vascular System
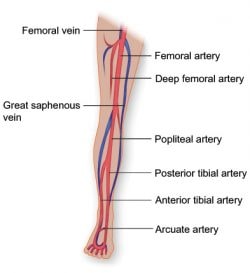
The vascular system comprises arteries, veins, and capillaries that transport blood throughout the body. Healthy veins have valves that prevent blood from flowing backward.
In cancer patients, the impact on the vascular system can be profound, potentially leading to vein damage and varicose veins as these valves weaken. This depends on the type of cancer and the stage.
Certain cancers are more well known to be a challenge for veins, as some product prothrombotic proteins that can contribute to developing a blood clot or blood clots in their veins resulting in deep vein thrombosis.
4. Symptoms of Varicose Veins in Cancer Patients
Varicose veins can cause a range of symptoms, including bulging veins, aching pain, and swelling. Cancer patients may notice these symptoms more acutely due to their overall health condition.
Additionally, they might experience skin discoloration and itchy skin around the affected veins. At times there are ulcers, known as venous leg ulcers (VLU) or bleeding from varicose or spider veins.
Occasionally, one can have a varicose vein with blood clots in it, known as superficial vein thrombophlebitis (SVT).
5. Risk Factors for Developing Varicose Veins
Several risk factors can increase the likelihood of developing varicose veins in cancer patients. Some patients simply have a family history of venous disease or superficial vein issues.
Others have experienced prolonged periods of immobility due to cancer treatment regimens including surgery or radiation therapy, the effects of chemotherapy drugs on blood flow, and the presence of a history of vein disease prior to cancer treatment.
Overweight and obesity can also exacerbate vein issues by putting added pressure on the vascular system. In all cases, there are weak or damaged valves that leads to pressure in the leg veins and blood vessels leading to chronic venous insufficiency.
6. Blood Clots and Varicose Veins
Cancer patients are at a higher risk of blood clots, which can complicate varicose veins. Blood clots may form in the veins, leading to conditions such as deep vein thrombosis (DVT) or pulmonary embolism.
7. Diagnosis and Monitoring
Diagnosing varicose veins in cancer patients involves a comprehensive understanding of their medical history and current condition. Doctors may use imaging techniques, such as ultrasound, to assess the health of the veins and detect any blood clots. Regular monitoring is crucial to manage vein health effectively.
8. Treatment Options for Varicose Veins
Treatment options for varicose veins in cancer patients vary based on the severity of the condition. Common treatments include wearing compression stockings to improve blood flow by preventing blood pooling in the lower legs.
Traditional varicose vein treatment options such as laser therapy or sclerotherapy for spider veins or ablation or surgical procedures to remove or close affected veins are not generally done when a patient is actively undergoing treatment for cancer.
However, once the treatments are over, or if a patient goes into a chronic phase without active chemotherapy, radiation or planned surgery, varicose veins treatments like RFA, Venaseal, Varithena, phlebectomy or sclerotherapy can be considered.
9. Managing Symptoms and Improving Quality of Life
Managing symptoms of varicose veins can significantly improve the quality of life for cancer patients. Approaches include elevating the legs, staying active within the limits of their condition, and using prescribed medications. Addressing vein health proactively can help alleviate symptoms such as aching pain and swelling. If there is a lot of swelling, as is sometimes seen with patients who have had radiation of lymph nodes or pelvic surgery, one can consider an intermittent pneumatic pump (IPC) to help reduce the swelling. If one develops venous leg ulcers, wound care and a vein treatment visit should be considered.
10. Seeking Medical Evaluation For Varicose Veins
Cancer patients experiencing varicose veins should seek medical attention to address both the veins and any potential complications if they have questions or concerns. Regular check-ups with healthcare providers can help them decide if and when a vascular evaluation is indicated. If there is any concern about a blood clot, one should seek medical attention promptly.
Conclusion
While there is no direct link between varicose veins and cancer, it’s essential for individuals with venous disease who are undergoing cancer treatments to be aware of certain considerations. Varicose veins are swollen, enlarged leg veins caused by weakened valves that struggle to return blood to the heart against gravity. They do not cause cancer, nor are they a symptom of cancer. But again, patients can have both varicose veins and cancer and thus questions can arise that are important to consider.
Varicose veins and spider veins with symptoms in cancer patients can require careful attention due to the complex interplay between cancer, treatments, and vascular health. By understanding the risks, symptoms, and treatment options, patients and healthcare providers can work together to manage vein health effectively. With proper care, it’s possible to alleviate symptoms for patients with varicose veins being treated for cancer and improve their overall well-being.
While varicose veins and cancer are not connected, there is a connection between cancer and blood clots, such as deep venous thrombosis (DVT) or blood clots in varicose veins called supeficial thrombophlebitis. If you have concerns about a potential blood clot, don’t hesitate—seek medical attention promptly.
Seek an Evaluation if you have more questions
Caner patients who have concerns about varicose veins and spider veins should engage in open communication with their healthcare providers especially regarding:
- Venous Thromboembolism (VTE) Risk: Cancer and its treatments can increase the risk of developing blood clots, including deep vein thrombosis (DVT) and pulmonary embolism (PE). Although varicose veins themselves don’t cause cancer, untreated vein disease can lead to blood clots. Therefore, patients with varicose veins should be vigilant about any signs of VTE.
- Vascular Ultrasound: In cases where a patient has varicose veins or suspected clot-related issues, a vascular ultrasound can help establish a diagnosis. It provides detailed images of blood flow and identifies any abnormalities in the veins.
- Treatment Timing: Generally, we avoid treating varicose veins when a patient is actively undergoing cancer treatment. However, it’s always an option to consult with a specialist to discuss treatment choices and understand what to expect in the future if the patient P should always consult their oncologist if they suspect a vein or vascular evaluation is needed. Open communication ensures the best approach to managing both cancer and vein health
Inovia Vein Specialty Centers:
Contact Inovia Vein today to learn more about the subject of varicose veins and cancer. We have 6 locations and have experienced doctors who can meet with patients, even those undergoing cancer treatments to help them understand their treatment options.